- How Does the CAD Technology Work?
- Studies with CAD Technology
- Benefits and Limitations of CAD Technology
Computer-aided detection (CAD) technology is a recent advance in the field of breast imaging. The CAD technology basically works like a second pair of eyes, reviewing a patient's mammogram film after the radiologist has already made an initial interpretation. If the computer software detects any breast abnormalities or "regions of interest" on the mammogram film, it marks them. The radiologist can then go back and review the mammogram film again to determine whether the marked areas are suspicious and require further examination (with additional imaging tests or biopsy). With the CAD technology, the radiologist still makes the final interpretation of the mammogram.
Based on clinical studies of the CAD technology, researchers estimate that for every 100,000 breast cancers currently detected with screening mammograms, the CAD technology could result in the detection of an additional 20,500 breast cancers.
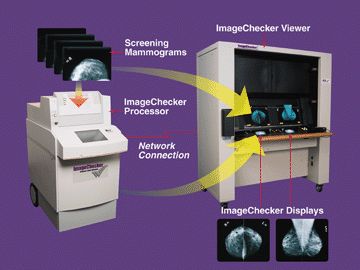
Photo courtesy of R2 Technology, Inc.
Mammography can help detect breast cancer at an early stage, when the chances for successful treatment and survival are the greatest. While mammography detects approximately 85% to 90% of breast cancers, mammogram films can be difficult for radiologists to read. Thus, radiologists can occasionally overlook breast cancers that are present on mammogram films. The CAD technology works as a "second reading" for radiologists, alerting them to areas on films that may require more attention.
Recently, Congress passed the "Medicare, Medicaid, and SCHIP Benefits Improvement and Protection Act of 2000" that will provide additional reimbursement for screening mammograms using the CAD technology. According to California Representative Anna Eschoo, this legislation will give women greater access to more accurate mammograms.
In essence, the CAD technology works like a "spell-checker." The computer marks abnormalities on the digitized films similar to the way a computer program might alert a writer to a misspelled word. After reviewing the computer’s marking, the radiologist can decide whether the marked area is indeed an abnormality that needs follow-up or if the computer has alerted him or her to a normal area, such as a blood vessel, that is no cause for concern. The final interpretation is still made by the radiologist.
To use the CAD technology, mammogram films are first loaded into a special processing unit that digitizes the mammogram images. The CAD unit then highlights any detected breast abnormalities on the digitized mammograms using special pattern recognition computer software. The digitized mammogram files are then transmitted to monitors on a motorized film viewer so the radiologist can compare the original film to the digitized mammogram image on the small monitor.
In the meantime, the radiologist reviews the patient’s original mammogram films and makes his or her interpretation as to whether any breast abnormalities are present (and whether they are cause for concern). After the radiologist finishes analyzing the mammogram films, he or she can view the digitized mammograms on the small monitor to determine whether the computer marked any abnormalities on the films. Based on the results of the CAD marker information, the radiologist may choose to re-examine the original mammogram films and modify his or her interpretation when appropriate.
Using sophisticated pattern recognition computer software, the CAD technology is designed to detect the following abnormalities on mammogram films:
- Patterns of bright spots that suggest microcalcifications (tiny calcium deposits that may indicate cancer)
- Dense regions with or without radiating lines that suggest breast masses or distortions
 |
The CAD system marks suspicious areas on the digitized mammogram film. Photos courtesy of R2 Technology, Inc. |
The CAD technology marks breast abnormalities on digitized mammography films using a special coding system. For example, the R2 Imagechecker marks clusters of calcifications with a small triangle and breast masses with an asterisk. (See the mammogram image below). CAD marks are only made on the digitized mammograms; the original films are not altered.
Several clinical trials evaluated the safety and effectiveness of the CAD technology prior to FDA approval of the R2 Imagechecker in June 1998. In one clinical trial, 12 breast centers (including several academic medical centers) provided case data to determine the sensitivity of the computer algorithms. In that study, mammogram films on which cancer was detected were submitted along with the patients' past "normal" mammogram films from the previous nine to 24 months ("normal" means that no breast abnormalities were noted). After digitizing the past "normal" mammogram films with the CAD technology, the computer-assisted system was able to detect 90% of cancers in the cases where cancer was overlooked by the radiologist.
A growing amount of research suggests that CAD may be useful in helping radiologists detect breast cancer on mammography films. In a review of several studies published in the April 2002 issue of the journal, Technology in Cancer Research and Treatment, Stephen A. Feig, MD, of the Mount Sinai Hospital in New York found that CAD can help radiologists spot breast cancer on mammogram films, particularly if the cancer is associated with calcifications (calcium deposits). Dr. Feig also concluded that the use of CAD does not appear to increase the risk of false positives. In other words, CAD does not appear to result in women having to undergo unnecessary additional breast cancer screening because of an incorrect reading by CAD technology.
A study presented at the 2000 Radiological Society of North America (RSNA) meeting found that using CAD technology can increase the detection of breast cancer by approximately 20%. Among the 12,860 women in the study, 49 cancers were detected:
- 32 cancers were detected by both CAD technology and by the radiologist, who interpreted the women's regular mammogram films
- nine cancers were detected by the radiologist alone
- eight cancers were detected by the CAD technology alone (the radiologist then reviewed the mammogram films again to find the suspicious areas)
However, some research has suggested that CAD is more helpful to radiologists with less experience interpreting mammogram films. In a 2005 study published in the European Journal of Radiology, researchers found that CAD was able to correctly point out cancers that junior radiologists tended to miss more often than for senior radiologists, who were more likely to correctly find breast cancer on mammography films than their junior colleagues. The researchers conclude that CAD may be an important educational tool as radiologists gain experience with mammogram films.
When applied to the United States population, researchers have estimated that for every 100,000 cancers currently detected with screening mammograms (in women with no obvious signs of breast cancer, such as a lump), the use of CAD technology could result in the detection of an additional 20,500 breast cancers. Detecting breast cancer at an early stage increases the chances of successful treatment and survival. For example, the five-year survival rate for ductal carcinoma in situ (DCIS), a type of early-stage breast cancer that is confined to the milk ducts of the breast, is nearly 100% with proper treatment.
Many physicians believe that CAD will become more widespread in the coming years as more mammography facilities acquire digital mammography and CAD technology. Right now, using the CAD technology requires facilities to devote a great deal of time (four to five minutes per case) and effort to digitize the films (at some facilities, an additional employee may be needed just to digitize the mammography films). The widespread use of digital mammography would increase efficiency because the films would already be digitized.
Some radiologists also believe that the CAD technology tends to sometimes mark a fairly high number of "normal" areas on mammograms as abnormalities. This may lead to the ordering of additional unnecessary and costly breast imaging and/or biopsies. Prior to the FDA’s approval of the R2 Imagechecker, clinical trials did not see a statistically significant increase in additional breast imaging at centers using the CAD technology. However, additional studies will continue to evaluate the advantages and disadvantages of the CAD technology.
In addition, the high cost of the CAD technology may hinder its widespread use. A CAD system costs approximately $200,000, in addition to the cost of a mammography system. The cost of CAD technology may also raise the price of mammograms for patients who receive the exams by $10 to $15 per exam.
Several companies are developing CAD systems and software to provide radiologist with the technology to help them interpret mammogram films:
- Imagechecker CAD system, made by R2 Technology - FDA approved
- CAD MammoReader software, made by ICAD, Inc. - FDA approved
- MammoReader CAD system, made by ISSI, Inc. - FDA approved
- Mammex Tr made by Scanis, Inc.
|
|
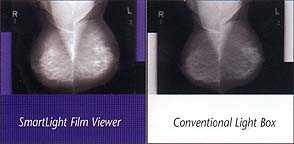
| By masking background light, the breast image becomes sharper and easier to interpret by using the digital film viewer on the left. Image courtesy of Smartlight, Inc. |
The FDA has also approved the Digital Film Viewer which can help radiologists when interpreting mammography films by blocking out the surrounding light on the films. By masking background light, the breast image becomes sharper and easier to interpret. In a large study, 1,027 radiologists agreed that using the Digital Film Viewer significantly improves visibility when reading mammogram films.
Using the Digital Film Viewer, the average radiologist is able to detect 30% to 60% smaller diameter objects compared to a normal light box. This reduces the likelihood that radiologists will overlook a small suspicious area on a mammogram film. As with CAD technology, the Digital Film Viewer technology may help radiologists to detect breast cancer at an early stage when the chances for successful treatment and survival are higher.
- The June 3, 2003 Imaginis report, "FDA Approves Computer-Aided Detection of Breast Cancer on Mammograms," is available at http://www.imaginis.com/breasthealth/news/news6.03.03.asp
- R2 Technology, Inc. the maker of the R2 Imagechecker for computer-aided detection of mammography provides information on CAD at http://www.r2tech.com/
- The November 30, 2000 Imaginis report, "Computer-Aided Detection Technology May Help Improve Accuracy of Mammograms," is available at http://www.imaginis.com/breasthealth/news/news11.30.00.asp
- SmartLight, Inc., the manufacturer of the Digital Film Viewer, provides information on the product at http://www.smartlight.com/
- To learn more about mammography, please visit http://www.imaginis.com/breasthealth/mammography.asp
Updated: May 4, 2008