A mammogram report is a key component of the breast cancer diagnostic process. While a mammogram cannot determine whether a woman has breast cancer, it may indicate whether a breast abnormality is present, and if so, it may characterize that abnormality. Further breast imaging (with spot views or ultrasound) or breast biopsy is usually a direct result of mammography findings.
This section describes information and terminology that may appear on a mammogram report. Please note, the organization and information contained on individual mammogram reports varies significantly. Some radiologists document every finding whether it is significant or not while others will only address important findings that warrant further examination. This section should only be used as a general reference for mammogram terminology and information that may be documented.
The actual mammogram report should not be confused with the report a woman is required by federal law to receive within 30 days of her mammogram. The latter is not a copy of the official radiology report, but rather, it is usually a short letter stating whether her mammogram was normal or if an abnormality was detected. If a patient does not receive written results of her mammogram within 30 days, she should call the facility where the exam was performed. She should not assume the results are normal. Click here for more information on the Mammography Quality Standards Act created by the U.S. Food and Drug Administration (FDA).
The following sections may be included in a mammogram report:
Patient information: Usually appears at the top of the report and typically includes the patient’s name, age, and the reason for the mammogram (i.e., annual screening mammogram, referred by physician to evaluate new right breast lump).
Clinical history: The patient’s medical and family history of breast cancer or other breast conditions. It may also include relevant medications the patient is taking, such as hormone replacement therapy.
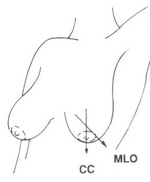
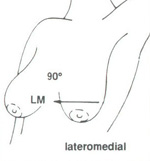
Procedure(s): May explain what types of mammogram views were taken. Typical views for screening mammograms include the cranio-caudal view (CC) and the medio lateral oblique view (MLO). Typical views for diagnostic mammograms include CC, MLO, and supplemental views tailored to the specific problem. These can include views from each side (latero medial, LM: from the side towards the center of the chest and mediolateral view, ML: from the center of the chest out), exaggerated cranial-caudal, magnification views, spot compression, and others.
 |
 |
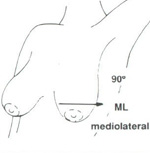 |
| Cranio-caudal (CC) view and mediolateral oblique (MLO) mammographic view | Latero medial (LM) mammographic view | Medio lateral (ML) mammographic view |
Impression: The radiologist’s overall assessment of the findings. Often includes a classification of the mammogram using the BI-RADS system developed by the American College of Radiology (ACR).
Recommendation (optional): Some radiologists may give specific instructions on what actions should be taken next. For example, the radiologist could recommend: no action necessary, a six month follow-up mammogram, spot views, breast ultrasound, biopsy, etc.
*See terminology section below for explanations of these terms
The following are terms may be found on a mammography report:
- Microcalcifications: Tiny calcium deposits less than 1/50 of an inch in size. When many microcalcifications are seen in one area, they are referred to as a cluster and may indicate a small cancer. About half of the cancers detected by mammography appear as a cluster of microcalcifications. Microcalcifications are the most common mammographic sign of ductal carcinoma in situ (DCIS), cancer that has not spread into neighboring breast tissue). Almost 90% of cases of DCIS are associated with microcalcifications.
- Macrocalcifications: Larger, coarse calcium deposits that are often related to benign (non-cancerous) growths such as fibroadenomas or with degenerative changes in the breasts, such as aging of the breast arteries, old injuries, or inflammation. Macrocalcifications are usually associated with benign (non-cancerous) conditions and may not require a biopsy. They are found in one out of two women over the age of 50.
- Dense, Density: Describes breast tissue that has many glands close together. Density shows up as a white area on a mammogram film. Though fairly common (especially in younger women), dense breasts may make microcalcifications and many other masses difficult to detect.
- Asymmetry: An area that is not found to be identical in both breasts (such as density). It is often a normal variant but can also be a sign of an abnormal growth.
- Cyst, Cystic or Simple Cyst: A fluid-filled mass. Simple cysts are benign (non-cancerous). Ultrasound is often used to confirm the presence of a cyst. Sometimes, cysts are drained with a fine needle aspiration biopsy.
- Monomorphic: Of the same shape. Monomorphic often describes microcalcifications that are uniform in shape and density (and usually non-cancerous).
- Pleomorphic, Polymorphic or Multiform: Having an irregular shape or various shapes. These terms often describe microcalcifications which can indicate ductal carcinoma in situ (DCIS), an early stage breast cancer.
- Lesion: A wound, injury, or other damage to a body part. Breast tumors are often referred to as lesions.
- Spiculated: On a mammogram, dense regions with radiating lines that suggest breast masses or distortions. The term is used to describe highly suspicious masses that may indicate cancer. However, some post-operative scars may be quite spiculated and resemble cancer.
- Mass, Lump or Nodule: A structure that can be felt when the breast is examined. Usually further evaluated with mammography and/or other breast imaging tests.
- Radiodense, Radiopaque: Effective in blocking x-rays. Breast tissue in younger women is usually more "radiodense" than the fattier tissue in older women. Some contrast agents used in various x-ray procedures are also radiodense.
- Palpable: A breast lump that can be felt by hand.
- Suspicious: A breast abnormality that may indicate breast cancer. On a mammogram, these abnormalities may be lesions such as spiculated masses or pleomorphic microcalcifications. (see above for definitions of these terms)
- Parenchyma, Parenchymal: The functional tissue of an organ. In the breast, it is the glandular tissue (as opposed to fatty or stromal (connective) tissues).
- Bilateral: Occurring on or in both breasts.
- Unilateral: Occurring on or in only one breast.
- Spot view (or compression mammogram, spot view, cone view, or focal compression view): Applying the compression to a smaller area of tissue using a small compression plate or cone. By applying compression to only a specific area of the breast, the effective pressure is increased on that spot. This results in better tissue separation and allows better visualization of the small area in question. Spot compression views show the borders of an abnormality or questionable area better than standard mammography views. Some areas that look unusual on standard mammography images are often shown to be normal tissue on spot views. True abnormalities usually appear more prominently and the margins (borders) of the abnormality can be better seen on compression views. Click here to learn more about spot view.
- Magnification views: Uses a small magnification table (depending on type of mammography system being used by the facility) to bring the breast closer to the x-ray source and further away from the film plate. This allows the acquisition of "zoomed in" images (2 times magnification) of the region of interest. Magnification views provide a clearer assessment of the borders and the tissue structures of a suspicious area or a mass and are often used to evaluate microcalcifications. Click here to learn more about magnification views.
- To learn more about mammography, please visit http://www.imaginis.com/breasthealth/mammography.asp
Updated: December 2010



