- Related Articles
- What is Mammography?
- How is Mammography Performed?
- Views Taken During Screening and Diagnostic Mammography
- Breast Compression During Mammography
- Minimizing Pain and Discomfort During Mammography
- Skin Markers During Mammography
- Special Mammography Techniques:
- Additional Information on Mammography

Technologist positioning a woman for Cranio-caudal (CC) view mammography
- Frequently Asked Questions About Mammography
- How Mammography is Performed: Imaging and Positioning
- Mammography on Small Breasts
- Keys Steps For An Optimal Mammogram
- Understanding the Mammography Report
- Find a Mammography Facility
- Choosing a Mammography Facility
Mammography is a special type of x-ray imaging used to create detailed images of the breast. It is estimated that 48 million mammograms are performed each year in the United States. Mammography uses low dose x-ray; high contrast, high-resolution film; and an x-ray system designed specifically for imaging the breasts. Successful treatment of breast cancer depends on early diagnosis. Mammography plays a major role in early detection of breast cancers. The US Food and Drug Administration reports that mammography can find 85 to 90 percent of breast cancers in women over 50 and can discover a lump up to two years before it can be felt. The benefits of mammography far outweigh the risks and inconvenience.
Mammography can show changes in the breast well before a woman or her physician can feel them. Once a lump is discovered, mammography can be key in evaluating the lump to determine if it is cancerous. If a breast abnormality is found or confirmed with mammography, additional breast imaging tests such as ultrasound (sonography) or a breast biopsy may be performed. A biopsy involves taking a sample(s) of breast tissue and examining it under a microscope to determine whether it contains cancer cells. Many times, mammography or ultrasound is used to help the radiologist or surgeon guide the needle to the correct area in the breast during biopsy.
There are two types of mammography exams, screening and diagnostic:
- Screening mammography is an x-ray examination of the breasts in a woman who is asymptomatic (has no complaints or symptoms of breast cancer). The goal of screening mammography is to detect cancer when it is still too small to be felt by a woman or her physician. Early detection of small breast cancers by screening mammography greatly improves a woman's chances for successful treatment. Screening mammography is recommended every one to two years for women once they reach 40 years of age and every year once they reach 50 years of age. In some instances, physicians may recommend beginning screening mammography before age 40 (i.e. if the woman has a strong family history of breast cancer). Screening mammography is available at a number of clinics and locations.
- Diagnostic mammography is an x-ray examination of the breast in a woman who either has a breast complaint (for example, a breast lump or nipple discharge is found during self-exam) or has had an abnormality found during screening mammography. Diagnostic mammography is more involved and time-consuming than screening mammography and is used to determine exact size and location of breast abnormalities and to image the surrounding tissue and lymph nodes. Typically, several additional views of the breast are imaged and interpreted during diagnostic mammography. Thus, diagnostic mammography is more expensive than screening mammography. Women with breast implants or a personal history of breast cancer will usually require the additional views used in diagnostic mammography.
During mammography, the technologist will position the patient and image each breast separately. One at a time, each breast is carefully positioned on a special film cassette and then gently compressed with a paddle (often made of clear Plexiglas or other plastic). This compression flattens the breast so that the maximum amount of tissue can be imaged and examined.
At some facilities, mammography technologists may place adhesive markers to the breast skin prior to taking images of the breast. The purpose of the adhesive markers is twofold: first, to identify areas with moles, blemishes or scars so that they are not mistaken for abnormalities, and secondly, to identify areas that may be of concern (e.g. a lump was felt during physical examination). Some centers routinely mark the nipple with a small dot to provide a clear "landmark" for the radiologist on the mammogram images. See the section below on skin markers for more information.
To "take" a mammogram, the x-ray source is turned on and x-rays are radiated through the compressed breast and onto a film cassette positioned under the breast. The x-rays hit a special phosphor coating inside the cassette. This phosphor glows in proportion to the intensity of the x-ray beams hitting it, thus exposing the film with an image of the internal structures of the breast. Highly sensitive film and special x-rays are used for mammography to create the highest quality images at the lowest exposure.
The resulting "exposed film" inside the cassette is then developed in a dark room much like a regular photograph is developed. It is the special energy and wavelength of the x-rays that allow them to pass through the breast and create the image of the internal structures of the breast. As the x-rays pass through the breast, they are attenuated (weakened) by the different tissue densities they encounter. Fat is very dense and absorbs or attenuates a great deal of the x-rays. The connective tissue around the breast ducts and fat is less dense and attenuates or absorbs far less x-ray energy. It is these differences in absorption and the corresponding varying exposure level of the film that create the images which can clearly show normal structures such as fat, fibroglandular tissue, breast ducts, and nipples. Further, abnormalities such as microcalcifications (tiny calcium deposits), masses, and cysts are also visible.
The developed mammography films are then interpreted by a radiologist, who compares the new images of a woman's breast to each other and to previous mammograms a woman has had. The radiologist will look for shadows and patterns of tissue density to detect any abnormalities.
A mammogram is like a fingerprint; the appearance of the breast on a mammogram varies tremendously from woman to woman, and no two mammograms are alike. It is extremely helpful for the radiologist to have films (not just the report) available from previous examinations for comparison purposes. This will help the doctor to recognize small changes that occur gradually over time and detect a cancer as early as possible.
The breast is made of fat, fibrous tissue and glands. Breast masses (these include benign and cancerous lesions) appear as white regions on mammogram film. Fat appears as black regions on a mammogram film. Everything else (glands, connective tissue, tumors and other significant abnormalities such as microcalcifications) appear as levels of white on a mammogram.
As of April 28, 1999, a new version of the Mammography Quality Standards Law mandates that all women who have mammograms must be informed of the results in writing. However, if you have not been informed of your results within a week or so of your mammogram, do not assume they are normal. Follow up with your referring physician or healthcare provider who will provide you with the results.
If women have questions about mammography during the procedure, they should feel free to ask the mammography technologist. If women have questions about their mammogram report or the radiologist's letter about their mammogram, they should direct those questions to the radiologist.
Detailed information on mammography positioning and imaging.
For screening mammography each breast is imaged separately:
- typically from above (cranial-caudal view, CC) and
- from an oblique or angled view (mediolateral-oblique, MLO)
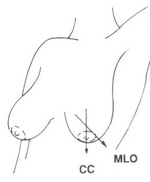
Cranio-caudal (CC) view and mediolateral oblique (MLO) mammographic view
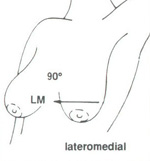
Latero medial (LM) mammographic view
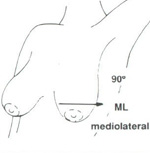
Medio lateral (ML) mammographic view
For diagnostic mammography, each breast is imaged separately:
- from above (cranial-caudal view, CC)
- from an oblique or angled view (mediolateral-oblique, MLO) and
- supplemental views tailored to the specific problem are often performed. These can include views from each side (lateromedial, LM: from the outside towards the center and mediolateral view, ML: from the center of the chest out), exaggerated cranial-caudal, magnification views, spot compression, and others.
- if screening mammography has been performed first and the resulting CC and MLO views are of sufficient quality, they may not need to be repeated if diagnostic mammography is required.
A cleavage view (also called "valley view") is a mammogram view that images the most medial (central) portions of the breasts. This is the portion of breast tissue "in the valley" between the two breasts. When one breast is imaged and the other breast is left out of the compression field, some of the breast being imaged may get pulled or left out too. To get as much medial tissue as possible, the mammogram technologist will place both breasts on the plate at the same time to image the medial half of both breasts.
A cleavage view may be performed when there is a questionable density on the medial edge of the mammogram film and the radiologist needs to see more of this density (if possible). A cleavage view may also be performed if the radiologist sees something suspicious in the mediolateral-oblique (MLO) mammogram view and cannot find the area on the cranial-caudal view (CC) view.
Detailed information on mammography positioning and imaging.
Breast compression is necessary to flatten the breast so that the maximum amount of tissue can be imaged and examined. Breast compression may cause some discomfort, but it only lasts for a brief time during the mammography procedure. Patients should feel firm pressure due to compression but no significant pain. If you feel pain, please inform the technologist. During the mammography examination, breast compression should only be applied two to four times per breast for a few seconds each time (see below for description of views taken during screening and diagnostic mammography).
Breast compression is necessary during mammography in order to:
- Flatten the breast so there is less tissue overlap for better visualization of anatomy and potential abnormalities. For example, inadequate compression can lead to poor imaging of microcalcifications, tiny calcium deposits that are often an early sign of breast cancer.
- Reduce overlapping normal shadows, which can appear as suspicious regions on the film.
- Allow the use of a lower x-ray dose since a thinner amount of breast tissue is being imaged
- Immobilize the breast in order to eliminate image blurring caused by motion
- Reduce x-ray scatter which also leads to image degradation
Some mammography facilities will allow the patient to control the breast compression herself during mammography.
The benefit of mammography in helping to detect breast cancer early clearly outweighs the temporary discomfort of the exam. However, some women do find mammograms to be uncomfortable and sometimes painful. Several studies over the last 10 years have isolated a number of factors that influence a woman's comfort level during mammography. These factors include:
- Breast compression
- Friendliness and sensitivity of the mammography technologist(s)
- Facility atmosphere and procedures
By surveying women about their experiences with mammograms, researchers offer suggestions on how to minimize discomfort during mammography.
To alleviate much of the pain associated with mammography, patients may wish to:
- Find a "friendly" mammography facility with knowledgeable mammography technologists
- Control the breast compression themselves during mammography
- Change mammography facilities when dissatisfied with care/service
- Use calming self-statements and learn distraction techniques to use during mammography
Some mammography facilities will allow the patient to control the breast compression herself during mammography. This can greatly reduce anxiety, making the woman feel more comfortable during the procedure, both physically and emotionally. Women should feel free to ask the technologist about controlling breast compression themselves when scheduling the exam or before the exam begins.
Researchers have found that a woman often feels more comfortable during a mammogram with a courteous technologist who can provide thoughtful answers to her questions. Knowledgeable technologists can also help women with distraction techniques to take their minds off the exam. In a study published in the February 2000 issue of the journal Radiology, researchers found that factors associated with mammogram discomfort included the facility itself, satisfaction with care, and the patient's perception of the technologist's "roughness."
If women are not satisfied with the quality of care they receive at one facility, they should feel free to change facilities. However, it is important that a patient obtain her original mammogram films if she changes facilities so that future films may be compared to them. Learn more about minimizing pain and discomfort during mammography.


Images Courtesy of Beekley Corporation
Many mammography facilities now use skin markers to help radiologists readily identify the nipple, surgical scars, raised moles, or other normal features on the breast. These markers are placed on the patient's breast skin before her mammogram and can easily be identified on the patient's resulting mammogram films. Markers may also be used to alert the radiologist to a breast abnormality that warrants close examination, such as a lump. The markers are either opaque or see-through and come in a variety of different shapes that correspond to different features on the breast. For example, the Beekley skin marker system uses a small pellet marker to indicate the nipple, a triangular marker to indicate a worrisome lump or mass, an S-shaped marker to indicate surgical scars, and a circular marker to encircle raised moles on the breast. The markers are made in such as way so they do not obscure any breast tissue.
By immediately identifying normal or worrisome areas of the patient's breast, the markers help save the radiologist time and confusion when reading the patient's mammogram film. Many physicians believe these markers are more useful than solely noting moles or other features on mammogram sketches because the shape of the breast is altered when it is compressed during the mammogram exam. Thus, the resulting films may not show a mole in the same area as noted by the technologist on a mammogram sketch. Nipple markers are especially useful because they help the technologist position the patient and verify that the nipple is in profile before the exposure is taken. The markers use adhesive similar to a Band-Aid and are easily removed after the mammogram.
In some cases, special mammography techniques are used to make a small area of breast tissue or a suspected abnormality easier to evaluate. Depending on the type of abnormality and its location in the breast, one of these special mammography techniques (spot compression and magnification views) maybe used.
More information on special mammogram views.
Imaginis provides several other articles on mammography to help women understand all aspects of the exam. Click on one of the links below for additional information on mammography:
- Screening Mammography
- Diagnostic Mammography
- Frequently Asked Questions About Mammography
- How Mammography is Performed: Positioning and Imaging
- Benefits of Receiving a Mammogram
- Key Steps for an Optimal Mammogram
- Mammography Preparation and What to Expect During Mammography
- Sample Pre-Mammography Questionnaires
- Special Mammography Views
- Mammography on Small Breasts
- Understanding the Mammogram Report
- Mammography Interpretation (ACR-BIRADS system)
- Finding a Mammography Facility
- Choosing a Quality Mammography Facility
- The Case for Mammography
- Advances in Mammography and Breast Imaging
- Digital Mammography
- Computer-Aided Detection Mammography



